Microgravity is known to put the wounds of astronauts at higher risk of scarring, but scientists don’t know why. Engineers are sending an experiment up into orbit to find out.
Within a couple of years, if all goes to plan, a little box will go 250 miles up in a rocket bound for the International Space Station. Described by NASA as the world’s “orbiting laboratory,” the space station holds more than 180 instruments and facilities to support scientific research. The box, smaller than most carry-on bags and described by Virginia Tech engineer Blake Johnson as an “experiment in a suitcase,” will join hundreds of ongoing investigations in those facilities.
Inside the box will be a self-contained, fully automated experiment, its valves turned wirelessly from Earth. And like a large slice of the studies onboard, the experiment will explore the effects of a condition unique to the International Space Station: microgravity. This near-total lack of gravity enables astronauts to float around as they send greetings to Earth, and it brings on the feeling of hanging upside down on monkey bars, astronaut Jessica Meir told NASA. But it’s also something that the human body hasn’t evolved to handle. Microgravity has been studied for its disruptive effects on vision, circadian rhythms, blood pressure, fluid flow, and bone density.

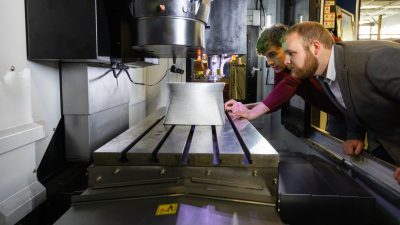
Through the workings of the little box, a team of engineers including Johnson, an associate professor in the Grado Department of Industrial and Systems Engineering at Virginia Tech, and Shayn Peirce-Cottler of the University of Virginia are studying microgravity’s effects on wound healing, an intricate series of steps in tissue regeneration that still puzzles scientists on Earth.
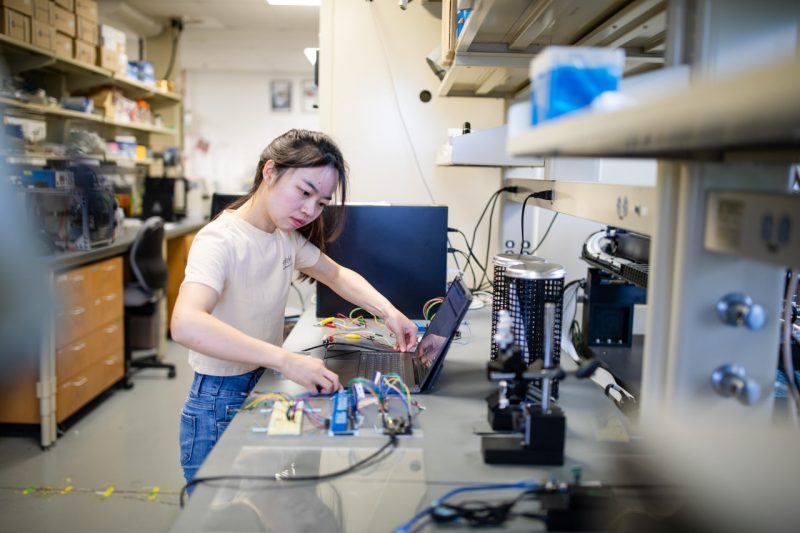
A delicate balance of space and time, wound healing is hypothesized to go haywire without gravity. To find out what happens to wound healing in space, the team will use a sensor-integrated 3D tissue culture model to follow microgravity’s effects on two key healing phases: blood vessel formation and tissue remodeling.
Meanwhile, on Earth, Peirce-Cottler’s lab will run the same experiment for comparison. “By doing experiments in both locations, we can make observations about the similarities or differences between how wounds heal in space versus on Earth,” Johnson said. “We want to use this fundamental understanding to create better technologies that can heal people’s wounds.”
Following a wound’s path over time — to either functional tissue or fibrosis, or scarring — could inform how we treat not only astronauts en route to Mars or the moon, but also people with fibrotic diseases on Earth. This potential impact earned the project joint support from the National Science Foundation and the Center for the Advancement of Science in Space, the NASA program that manages research and development for the International Space Station.
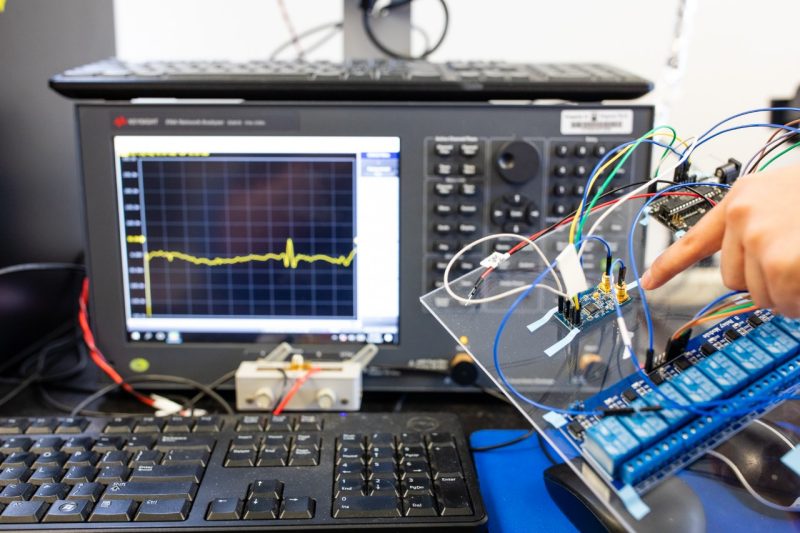
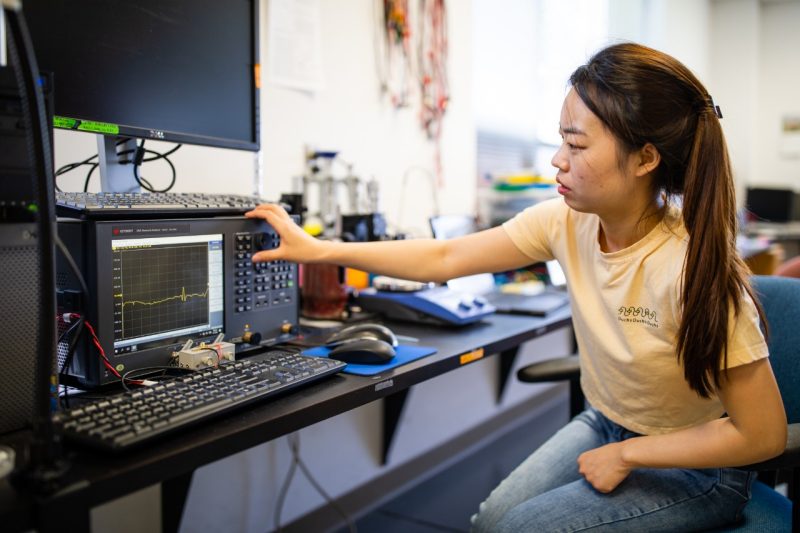
To measure the progress of wound healing processes, the experiment will include a sensor platform developed by Johnson, an expert in sensing and biomanufacturing. The sensors will enable biomedical engineers led by Peirce-Cottler to study wound healing dynamically, giving the project its “big innovation,” she said. That’s because Johnson’s sensor platform is one of the few mechanical testing tools that can precisely measure the “complex combination of requirements” involved in keeping wound healing on track — as well as the moments where it may go off the rails.
“With Dr. Johnson’s sensor technology and with live microscopy imaging, we can watch wound healing unfold, and watch it continuously, which is amazing,” Peirce-Cottler said. “That is so important. Because this process is essentially a conversation between cells that unfolds over time.”
A Goldilocks effect
Wound healing can generally be broken down into three phases, explained Peirce-Cottler, a professor of biomedical engineering and chair of the Department of Biomedical Engineering at the University of Virginia.
First, there’s inflammation. Inflammatory cells come in and “gobble up” dead or injured tissue and any bacteria in the wound. In the second, critical phase, the blood vessels grow in. They deliver oxygen and nutrients to the cells that will move in next to fill the space with functional tissue. Those cells are fibroblasts, responsible for the third phase of wound healing: once blood vessels settle down with their growth and regress if needed, fibroblasts are cued to begin tissue remodeling, which they do by laying down layers of collagen known as the extracellular matrix.
“All of these dynamic processes, it’s kind of like a Goldilocks thing,” Peirce-Cottler said. “We need just the right amount. Not too much, not too little, and it all has to be timed perfectly.”
To maintain this delicate balance, cells are in constant communication. Scientists have different theories for how these conversations go, how they go awry, and how microgravity stirs the pot, resulting in fibrosis. Fibrosis occurs when fibroblasts secrete excess collagen and other proteins that make up the extracellular matrix, stiffening the tissue. Microgravity is known to put astronauts at higher risk of this response, and Peirce-Cottler believes that it could be because microgravity disrupts the signals sent between blood vessel cells and fibroblasts, sending fibroblasts into overdrive.
“We think those fibroblasts are going to be hyperactive and get stimulated to produce more extracellular matrix than they are supposed to, and stiffen the tissue to the point where the blood vessels that are just trying to do their thing and keep everything under control, are also going to be screwed up,” Peirce-Cottler said. “We expect that there are going to be fewer blood vessels in total as a result, and the tissues are going to be stiffer. But we have no idea. The truthful answer is, it could go completely opposite. There’s so much untested, and until the development of sensor-based, experimental platforms like Blake’s, we’ve never had tools that would be able to measure these processes dynamically.”
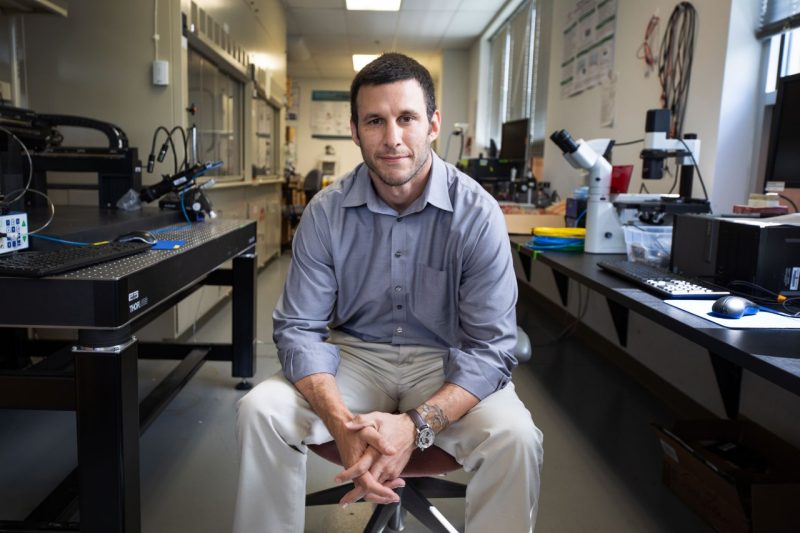
Johnson has spent much of his career exploring what’s possible with sensors, not only in terms of measuring something for the first time, as he’s enabling Peirce-Cottler’s lab to do here with tissue stiffness, but in pulling new techniques from data science and artificial intelligence into the field of sensing. In 2022, Johnson received a National Science Foundation Early Career Development (CAREER) Award for his work building sensors that can identify and quantify molecules in different environments with the help of machine learning.
“Sensing is in a continued growth phase,” Johnson said. “People are continuing to develop new tools and new sensors to measure things that haven’t been monitored before, while trying to make measurements faster, more resilient, and more reliable. It’s a really active and interdisciplinary field.”
More than just an ear to the door
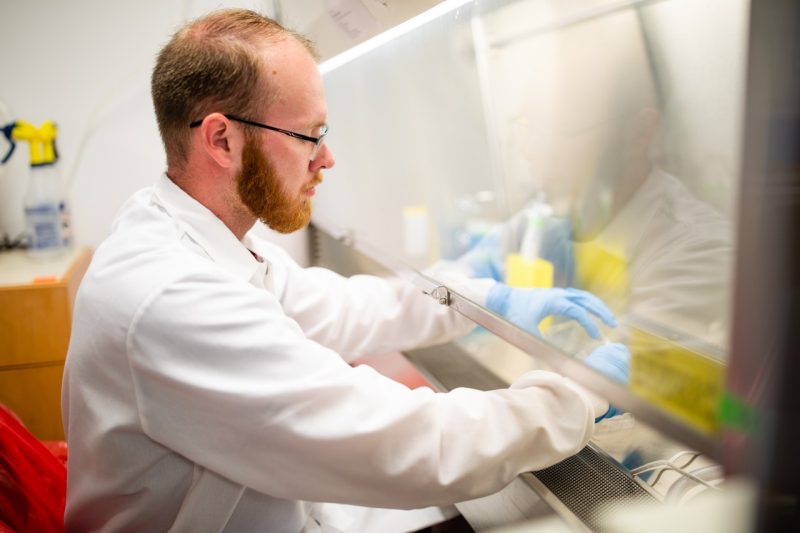
Inside the box aboard the International Space Station will be a tissue culture model — a simplified version of a wound, capturing the most important processes in wound healing — paired with Johnson’s sensor platform. For the model, a standard plastic well plate will be filled with gel, simulating the extracellular matrix. Fibroblasts will be suspended in the gel, with blood vessel cells on top. As artificial wound healing progresses, Johnson’s sensors, poking up from the underside of the wells, will measure the gel’s stiffness as it’s affected by microgravity. Using live imaging, the team will also monitor the blood vessel cells above, to see if they dissolve or instead form more blood vessels and connect to form a network in a lacy pattern, as they do in the human body.
The researchers will watch for any potential interplay between the tissue stiffness caused by the fibroblasts and the blood vessel activity above them. Because these cells are alive and communicating with one another, what happens will also change over time, Peirce-Cottler explained, which is why Johnson’s new sensor platform is so important to her. Johnson’s technology can noninvasively, nondestructively, and continuously measure tissue stiffness, while working with the well plates familiar to scientists.
With sensors, the platform can also measure extracellular matrix stiffening in new detail. Current tools for mechanically testing tissue involve sacrificing samples to get the data, which means the data represents the state of that tissue for just one moment in time. Johnson’s technology instead measures stiffness over hours and days, capturing any heterogeneities. “A lot of research questions are driven by methods that involve observation and measurement,” he said. “But a lot of those questions require you to monitor something continuously. And that requires a sensor.”
Returning to the idea of wound healing as a series of conversations between cells — and fibrosis as the result of those conversations devolving into miscommunication — Peirce-Cottler described traditional tools as a quick ear to the door, listening only briefly to cell conversations becoming arguments. Johnson’s sensors instead capture the full length of those conversations.
That makes for better data, Peirce-Cottler said. “When you’re listening to an argument, you can’t just put your ear to the door for five seconds and walk away,” she said. “You make assumptions that might be wrong. You need to come back 10 minutes later. Is it still going on? Having this dynamic monitoring of the conversations by imaging the cells and watching them interact with one another, while simultaneously measuring the mechanical environment, is exactly what we need to figure out: Where are these conversations going awry? What is happening in the environment to cause this ‘argument?’”

Set it and forget it
As one of hundreds of experiments taking place in the International Space Station, the team’s “experiment in a suitcase” is designed to be picked up, set down somewhere on board, and left to its own devices. To make the experimental setup space-ready, the researchers are relying on Space Tango, a Kentucky-based company specializing in automated science in space.
“We’re interested in creating fully autonomous experimentation methods because they can potentially provide high throughput with reduced need for human resources,” Johnson said. The experiment’s design of multiple wells attached to multiple sensors gives it that high-throughput quality. “In terms of making discoveries and doing high-throughput research with a good bang for your taxpayer dollar, there’s a lot of value in creating experiments that can run fully autonomously.”
The experiment will run for a few weeks, after which the box will fly back down to Earth on another rocket. Whatever the researchers discover from the measurements made will help them better understand the biological underpinnings of derailed wound healing, Peirce-Cottler said, not just with microgravity, but also with fibrotic diseases we don’t yet fully understand. “Diabetic wound healing is a kind of parallel story to what we think is happening in space,” she said. “With diabetes, the conversations between the blood vessel cells and the fibroblasts also go off the rails, leading to tissue stiffening and serious problems with the blood vessels.”

Johnson’s sensor system also has broader applications. The researchers believe that if they can pinpoint when and how excess tissue stiffening happens, they can find the right point at which to bring in a drug to intervene. Scientists could also use the tool’s high-throughput system to find the right drug. “We can better understand this coordination between cells as well as its sensitivity to the different drugs used to try to support wound healing processes,” Johnson said.
It would be like finding a therapist to step in before cell conversations turn into arguments, Peirce-Cottler said. “In a 96-well plate, you could have 96 different drugs that you’re screening to say, ‘OK, this drug is the one that’s going to make that conversation get back on track,’” she said. “This therapist walks in at just the right moment, redirects the conversation, and prevents bad fibrosis. Cells reconcile and cooperate to regenerate the tissue and heal the wound.”
This is how Johnson and Peirce-Cottler envision using his sensor platform in the future. But the path to translating scientific discovery into fixes for fibrosis begins with a busy little box in space.
Photos by Peter Means
If you want to have an impact on our students and faculty like those featured in this magazine, go here to support the College of Engineering. For more information, call (540) 231-3628.
-
Article Item
-
Article Item