A research team blends specialties in microbiology, water chemistry, and environmental engineering to chase strains of Legionella, the elusive waterborne bacteria that causes Legionnaires’ disease.
A search for the source begins — some place, or places, where Legionella meets water, meets air, meets a breath taken in. When virulent strains of the bacteria cause an outbreak of Legionnaires’ disease, communities and their public health officials take steps to rout them out from spots at the mouth of built water systems and the things those systems feed, like shower heads, faucets, ice machines, hot tubs, and cooling towers. By collecting and testing water samples from these spots, investigators can learn where virulent Legionella may have been lurking before escaping into the air in tiny drops of aerosolized water, infiltrating human lungs, and causing a respiratory illness that kills 1 in 10 infected.
Since 2000, the rate of reported Legionnaires’ disease cases has climbed by nearly nine times in the U.S. 2015 saw multiple outbreaks: In July, New York City’s worst-ever outbreak took place in the South Bronx. The city’s health department ultimately traced common exposures to a cooling tower on the roof of the Opera House Hotel, with investigators sampling 55 cooling towers from 46 buildings in the process. The same month, an outbreak began at the Illinois Veteran’s Home in the city of Quincy. Reports from the Centers for Disease Control and Prevention list dozens of sites sampled at the 210-acre campus, in another wide search: “Elmore East Tub Showerhead,” “Sunken Garden Pool,” “Markword Ice Chest.”
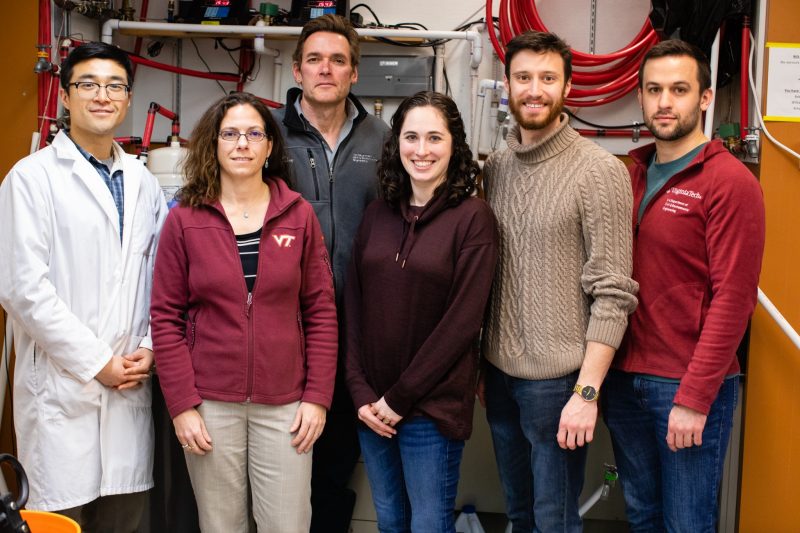
“It gives you an inkling of how pervasive water is in our environment, in our lives, and all the ways it can go wrong,” said Marc Edwards of the places where Legionella can hide. He and fellow Virginia Tech researcher Amy Pruden led a team in bringing an academic perspective to the state’s response in Quincy. Pruden, the W. Thomas Rice Professor in Engineering, and Edwards, the University Distinguished Professor of Civil and Environmental Engineering, have worked together to study Legionella since 2009, in research that more than once has taken their team into the midst and the wake of outbreaks.

Edwards, a water chemistry expert who has long focused on lead in water, is drawn to the study of Legionella for the mystery that still surrounds it.
“Lead is the oldest, best-known contaminant, whereas Legionella is brand new in the scientific scheme of things,” Edwards said. “There are ramifications in everything we do — everything we find.”
There’s a lot left to find. Scientists are still learning how the bacteria — naturally present in lakes, ponds, and even rain — grows in built water systems. They’re still trying to decipher its virulence — what makes some strains aggressive, while others remain relatively harmless. Legionella is likely to be detectable at trace levels all over the U.S., Pruden said, but it doesn’t always lash out through infection. Scientists are also still trying to figure out what we may be doing with our plumbing to favor the more virulent forms.
“From a scientific standpoint, it’s very fascinating; there’s so much to learn about Legionella,” said Pruden, a microbiologist and environmental engineer. “But from a standpoint of trying to protect public health, it’s very frustrating.”
Over the past decade, Pruden has worked with Edwards and their students to study Legionella as it operates before, during, after, and outside of Legionnaires' disease outbreaks. They've monitored the bacteria’s levels at baseline, laying low in homes, and its levels in well water before and after floods. They’ve tested ways to keep the bacteria at bay, such as probiotic treatments that harness good bacteria to crowd out Legionella. They’ve looked holistically at its life in water systems, examining how water’s journey from municipal suppliers to buildings affects its quality and could affect Legionella’s growth. That growth is typically an issue relegated solely to buildings and their problems with things like old pipes or stagnant water, Pruden said, but her team believes there may be more to it.
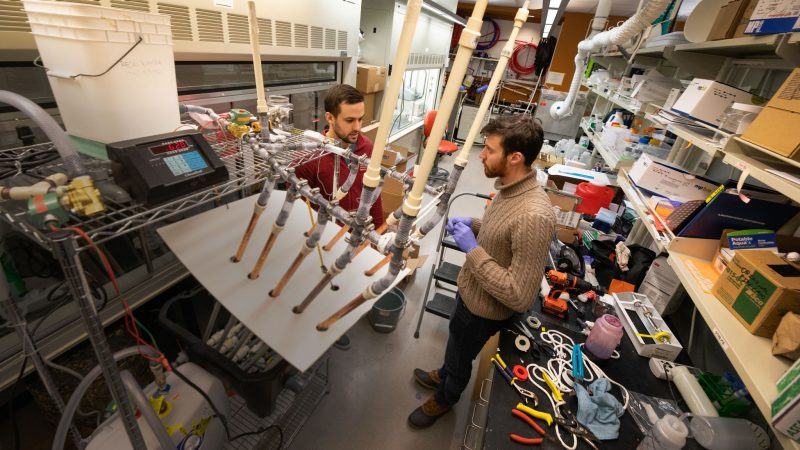
The researchers have also aimed to think holistically as they've investigated real-world Legionnaires' disease outbreaks in real time and for years afterward. In this area of their research, which has them working to piece together the conditions responsible for each outbreak, and others, they use methods like next-generation DNA sequencing and recreate real-world water systems in the lab.
In one of the team's latest published studies, after five years of fine-tuning and “probably almost a hundred failed experiments,” they were able to recreate and learn from water chemistry and Legionella growth trends associated with a pair of outbreaks in Genesee County, Michigan, Edwards said. There, Legionella crept in the shadow of a lead-in-water crisis.
‘We don’t need another problem’
In 2014 and 2015, two outbreaks of Legionnaires’ disease swept through Genesee County, Michigan, home to the city of Flint, and sickened at least 86 people, killing 10. The Michigan Department of Health and Human Services acknowledged being aware of the rising cases in late 2014 and supporting investigation and response thereafter. The department publicly reported the outbreak in January 2016.
Six months earlier, in July 2015, Edwards sat in a hotel room in Boulder, Colorado, between sessions of a microbiology conference, thinking about his next move. After Edwards had helped Flint resident LeeAnne Walters detect high lead levels in her family’s drinking water in April, his team and Walters had begun to mount a citizen science project that involved independently sampling and analyzing tap water for lead in 300 Flint homes. But he found it possible that lead contamination wasn’t the only issue.
Edwards remembers being afraid at the time that more might be going on since the city had switched its source of drinking water to the corrosive Flint River. Flint residents had mentioned skin infections and other symptoms that could be linked to bacteria in the water, he remembers. Though the local uptick in Legionnaires’ disease cases was not yet on his radar, Legionella came to mind. Edwards and Pruden had conducted research positing that exposure to a corrosive water supply could create conditions conducive to Legionella’s growth in buildings.
Pruden was at the conference with Edwards. He seemed preoccupied, she remembers, and he was constantly on the phone. She later learned he’d been talking to fellow Flint whistleblowers LeeAnne Walters and Miguel Del Toral. There was a problem with the water in Flint, Edwards eventually told her.
Edwards had been focused on the lead problem so far, but he told Pruden that residents had asked for testing for other things, too, like rash-causing bacteria. He asked her to bring a microbiological dimension to the investigation by helping his team test for potentially dangerous bacteria. The two and their students began to search for opportunistic pathogens in Flint, including Legionella pneumophila; Mycobacterium avium, a group of bacteria that can also infect the lungs; and Staphylococcus aureus and Pseudomonas aeruginosa, bacteria known to cause rashes. They tested for the pathogens among water samples from homes and businesses in small buildings, as well as the samples they’d already collected for lead testing.
At the same time, the researchers investigated possible links between Flint’s corrosive water supply switch and Legionella. They looked at a variety of the switch's effects; corrosive water had released iron in pipes, for instance, which is a key nutrient for Legionella and could have a role in its growth, Pruden explained. They also looked at the role of rapid decay of chlorine disinfectant resulting from corrosion.
At first, the team didn’t find much of any of the microbes they tested for, including Legionella. To Pruden, that was a good thing. “We don’t need another problem,” she remembers thinking. Meanwhile, the lead testing results came through and Edwards and then-graduate student Siddhartha Roy stood with Flint residents in a September press conference to share the jarring numbers, followed a few weeks later by pediatrician Mona Hanna-Attisha’s release of equally jarring results on blood-lead levels among Flint children. In October, officials announced that the city would switch its water source back to the Detroit River.
Edwards and Pruden remember that at that point, they still wanted to find out why there didn’t appear to be a problem with bacteria in the water, with the switch to a corrosive water supply. The team returned to Flint to look for Legionella in more places. They widened their search to large buildings, which with more extensive plumbing can be more supportive of the bacteria’s growth. This time, the Legionella levels they found were off the charts, Pruden said. They reported their findings to the state and the local health department.
The team kept the public updated on their lead and Legionella investigations at the Flint Water Study site. “People wanted to know what happened,” said Pruden. “You had the whole nation – the whole world’s – attention. As a scientist, I had known about problems with our water infrastructure for years, but most of the time, people don’t think about where their water comes from. Now, the public was suddenly very interested in what was going on with their water treatment and distribution, and there was this tremendous pressure to say something – but you also had to make sure you got it right.”
In early 2016, after the outbreaks had passed, Edwards and Pruden continued to study Legionella in that context. To them, working in real-world outbreak conditions could lead to scientific breakthroughs.
A post-mortem investigation
To unravel what may lead to an outbreak like the ones in Genesee County, the team has worked for the past five years from data collected in the field. They’ve done the same for Quincy. Fieldwork has supplied them with water samples and details from inspecting system conditions like pH, pipe material, flushing regimes, and flow rates. It’s also involved listening to water users and coaxing out observations big and small. “You talk to people who experienced the problem and used the plumbing,” Edwards said. “They’re living this unfortunate real-world experiment, and you have to get all the data possible from them.”



Pruden sees this second phase of research as a kind of post-mortem investigation. The team had one such study published by the Centers for Disease Control and Prevention’s Emerging Infectious Diseases in September 2019. Using 103 tap water samples gathered from Flint buildings in March, June, and August 2016, they used next-generation DNA sequencing, a specialty of Pruden’s, to examine Legionella strains that could have colonized local water systems in the months or years surrounding the 2014 and 2015 outbreaks.
They isolated and cultured Legionella pneumophila from the water samples – preparing what’s known as water isolates – and compared them genetically to clinical sputum isolates of Legionella pneumophila known to cause Legionnaires’ disease, specifically isolates sourced from phlegm coughed up by Legionnaires’ disease patients. The clinical sputum isolates were submitted to a Genesee County lab during the 2015 outbreak and passed on to the team for analysis by the state health department.
The researchers' use of next-generation DNA sequencing, specifically whole-genome sequencing, allowed them to pull up thousands of genes and probe differences in the genomes of individual strains. Whole-genome sequencing of both sets of isolates revealed a surprising amount of genetic diversity, Pruden said. Some of the water and clinical isolates were highly similar, but none were identical. Her team found that patients were infected with multiple strains of Legionella pneumophila and the tap water contained multiple strains as well. While a single strain connecting patients and water sources would have given the team clearer insights, the data didn’t show them one. To Pruden, that’s in line with Legionella’s elusiveness.
“This organism just doesn’t like to make things easy,” Pruden said.



Still, the team has made progress. In September 2020, they published their findings from recreating trends in water chemistry and Legionella proliferation observed in the field in Flint, when Flint River versus Detroit River water was used before, during, and after the 2014 and 2015 Legionnaires’ disease outbreaks. They found that the recreations showed growth and loss of Legionella pneumophila linking the outbreaks to an interplay of pipe materials in Flint premise plumbing, different flow patterns, and water chemistry changes tied to the switches in the city’s water supply at the time.
Such findings potentially broaden the scope of outbreak risk. The team looked not only at buildings, but at suppliers. To Edwards, the study is a capstone to their five years of experiments on Legionella in Flint. “This paper really starts to unravel the complexity of what happened in Flint, in terms of pipe material, lack of corrosion control, and even differences in mixing of water in large versus small buildings,” he said.
Studying Legionella today
New folds in the pathogen’s story continue to appear to the researchers. They believe the risk of Legionella may now be piggybacking on another crisis: the COVID-19 pandemic. When the pandemic triggered the rapid shutdown of buildings early on, the risk of Legionella and other waterborne pathogens growing in them, potentially flourishing in stagnant water during their inactivity, blew up to span the entire country.
With that major shift in water treatment, distribution, and use patterns comes the need for guidance, Pruden said. William Rhoads, one of her and Edwards’ Ph.D. students during the Flint and Quincy outbreaks and now a research scientist on their team, has focused on filling that need. Rhoads and several team alumni spoke to the issue, examined it in a May 2020 study, and continue to examine it.
Understanding how Legionella may evolve as a threat amid the COVID-19 pandemic will call on the same kind of holistic thinking that Rhoads and current and former team members have used before, Pruden believes.
“Through Flint, Quincy, and now COVID-19, we’re seeing that we need a more comprehensive framework for preventing the spread of Legionnaires’ disease, one that goes beyond a focus just on maintaining individual building water systems, and considers factors at play in the community water supply as well,” she said.
Some photos taken prior to onset of COVID-19 pandemic.
If you want to have an impact on our students and faculty like those featured in this magazine, go here to support the College of Engineering. For more information, call (540) 231-3628.
-
Article Item
-
Article Item
-
Article Item